THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT
85 year old female WITH Altered sensorium under evaluation
Hypoalbuminemia Anaemia under evaluation secondary to nutritional cause
Denovo dm and dcmp
-
CASE HISTORY
A 85 year old female , home stayer BY OCCUPATION ,CAME TO THE casualty WITH
CHEIF COMPLAINTS OF -
decreased sensorium since 4 days
Complains of Bowel and bladder incontinence since 4 days
patient was apparently asymptomatic 4 days back ago then he had history of irrelevant talks with her daughter at around 9:30 p.m. after dinner 4 days back
attenders thought it was due to her age next day morning patient got from bed had breakfast and at around 2 p.m.
while she was walking she had ? giddiness and fall on face followed by loss of consciousness for 10 minutes with no history of seizures head trauma ENT bleed
no history of nausea vomiting
She was taken to a local RMP then he said her Bp was low she was given IV fluids and injection diclofenac Im /stat
Next day morning attenders took her to hospital in Nalgonda CT brain was done which was normal and said to have low HB
HISTORY OF PRESENTING ILLNESS -
PATIENT WAS APPARENTLY ASYMPTOMATIC 4 DAYS BACK then while she was walking she had ? giddiness and fall on face followed by loss of consciousness for 10 minutes with no history of seizures head trauma ENT bleed
NO SIGNIFICANT PAST HISTORY , AND THEN CAME TO KIMS FOR FURTHER EVALUATION patient unable to roll on bed
bowel and bladder incontinence present
accepting feeds
PAST HISTORY -
NOT A KNOWN CASE OF HTN , DM , EPILEPSY , ASTHMA , TB
No previous surgical history
PERSONAL HISTORY :
DIET - MIXED ,APPETITE -normal appetite ,BOWEL MOVEMENT - REGULAR , BLADDER MOVEMENTS - REGULAR , ADDICTIONS(ALCOHOL AND SMOKING) - no addiction
FAMILY HISTORY -
Not significant
ON EXAMINATION -
PATIENT IS CONCIOUS , not orientation to time place person
PALLOR present,(no ICTERUS , CLUBBING , CYANOSIS , LYMPHADENOPATHY , EDEMA)
dehydration mild
VITALS -
TEMPERATURE - AFEBRILE
PULSE RATE - 60 BPM
BLOOD PRESSURE - 140 /70 MM OF HG
RESPIRATORY RATE - 14
SPO2 - 99% AT ROOM AIR
SYSTEMIC EXAMINATION -
CARDIOVASCULAR SYSTEM : S1 AND S2 HEARD , NO MURMURS
RESPIRATORY SYSTEM : BILATERAL AIR ENTRY PRESENT ,NORMAL VESICULAR BREATH SOUNDS
CENTRAL NERVOUS SYSTEM : Nad
pupils nsrl
gcs e2v1m2
Power only right upper limb moving 1/5
Tone hypotonic in all limbs
reflexes biceps triceps supinator knee qnkle
ul. 2+. -. -. -. -.
ll. 2+. -. -. -. -.
plantar bl mute
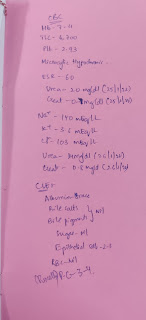
INVESTIGATION -
sr lipd profile,tyroid profile,ecg,haemogram,urine protein to creat ratio
TREATMENT GIVEN -
1 . IV fluids DNS NS at the rate of 30 ml per hour
2. Inject optineuron 1 ampule in hundred ml NS slow IV OD
3 .Inject pantop 40 MG IV OD
4. Rt feed 100ml milk fourth hourly 50 ml water 2nd hourly
5.Monitor vitals 4th hourly
6.Input output charting
7.BP monitoring second hourly
8 Grbs chatting fourth hourly




Comments
Post a Comment