THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT
36 YEARS OLD MALE WITH acute pancreatitis with alcohol dependence
-
CASE HISTORY
A 36 YEAR OLD MALE , driver BY OCCUPATION ,CAME TO THE casualty WITH
The case was driver in police department under rajakonda commistrate he worked as driver to asst commissioner of law and order division he used to work 24 hour shifts followed by of day of 24 hour period while on duty days he didn't used to drink
He previously had 2 episode of accident in past after drinking episode
1 st episode 10 years back after he drink at friend wedding while returning to home tossed of from bike over speed breaker and had bleeding from nose and mouth and injured toungue for which he needed stitches he was admitted in global hospital for 10 days stay
2 episode
He mis judged the cotton over loded lorry and feel from bike and had abrasion which heeled
In June 2020 he was framed by while he was working as driver for acp of ibrahimpatnem the local leader his friend given some paper for legal work with 2000 rs hidden in between which our pt delivered as a mediator to acp
and the acp got suspended immediately for taking bribery he got complainted by some staff member
and after 3 months
pt was framed by coworker whoes identity is not revealed by the government for safety that the driver also took bribe and he was suspended for 1 1/2 year span
There was some local st members function after suspension during which he consumed alcohol quantity not known by pt but in pt words he specify a lot after which he had very severe abdominal pain squeezing type for which he got admitted in drdo hospital and it got relieved and he was advised to cut down on drinking
Then he stopped drinking for a while then in August his friend mother died and at that function he consumed 300 ml whisky and again started drinking on weekly basis and during new year evening party with friends he consumed alcohol quantity not known in pt word he specify a lot and latter
He had abdominal pain again associate with sob even at rest and got admitted in Kims narketpally for further evaluation
CHEIF COMPLAINTS OF -
Complains pain in the epigastric region since three days dragging type
Complains of belching 2 to 3 times per day
no complains of nausea and vomiting complaints of decreased appetite
patient was apparently a symptomatic three days ago then he developed
complains of epigastric pain which is sudden in onset non-radiating type
no history of nausea vomiting
history of decreased appetite
no history of past surgery
No history of jaundice previously
no history of gallstones
history of epigastric pain six months back
constipation since 3 days
HISTORY OF PRESENTING ILLNESS -
PATIENT WAS APPARENTLY ASYMPTOMATIC 4 DAYS BACK then she developed fever SUDDEN ONSET associated with chills and rigors and headache (frontal and occipital) c/o sob since 4 days (grade 2 ) vomiting since 2 days back -1 episode food as content dragging sensation in leg since 4 days h/o back pain since 3 days NO SIGNIFICANT PAST HISTORY , AND THEN CAME TO KIMS FOR FURTHER EVALUATION NO H/O LOOSE STOOL
PAST HISTORY -
NOT A KNOWN CASE OF HTN , DM , EPILEPSY , ASTHMA , TB
No previous surgical history
no history of gallstones in the past
PERSONAL HISTORY :
DIET - MIXED ,APPETITE -Decrease appetite ,BOWEL MOVEMENT - irREGULAR Since 3 days, BLADDER MOVEMENTS - REGULAR , ADDICTIONS(ALCOHOL AND SMOKING) -
Alcoholics in seven years takes at least 150 ML
occasional toddy user also Since six months drinks 180 ML per Day
no history of smoking or chewing tobacco
brand used it is (Royal stag or IB )180 ML per Day is in six months
FAMILY HISTORY -
Not significant
ON EXAMINATION -
PATIENT IS CONCIOUS , COHERENT COOPERATIVE
NO PALLOR , ICTERUS , CLUBBING , CYANOSIS , LYMPHADENOPATHY , EDEMA
VITALS -
TEMPERATURE - AFEBRILE
PULSE RATE - 97 BPM
BLOOD PRESSURE - 100 /70 MM OF HG
RESPIRATORY RATE - 22
SPO2 - 98% AT ROOM AIR
SYSTEMIC EXAMINATION -
CARDIOVASCULAR SYSTEM : S1 AND S2 HEARD , NO MURMURS
RESPIRATORY SYSTEM : BILATERAL AIR ENTRY PRESENT ,NORMAL VESICULAR BREATH SOUNDS
CENTRAL NERVOUS SYSTEM : Nad
P/a -
Pain in the epigastric region and
pain is more in the right iliac and lumbar region
No bruit’s
negative Cullens sign and grey turners sign
Bowel sounds present
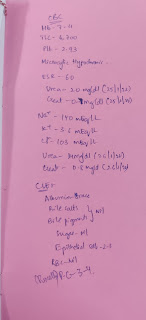
INVESTIGATION - haemogram,cue ,x-ray errect abdomen and xray chest pa,sr creatinine , electrolyte,lft,
Treatment GIVEN -
1 . Ivf ns and rl and dns @ 50 ML /hr
2. Ink . PANTOP 40 MG Iv/OD
3 .Ink zofer 4 mg IV sos
4. inj tramadol 1 amp in 100 ml na IV BD
5.inj buscopan 22 cc iv/sos
6.tab pcm 650 mg po/tid
7.grbs 6 th hourly
8 temp and i/o charting
clinical images


















Comments
Post a Comment